Haemodialysis
Haemodialysis
In haemodialysis, blood is purified with the help of dialysis machine and dialyzer.
How is haemodialysis done?
Most of the time, haemodialysis is performed in hospitals or free standing dialysis centres, under the care of doctors, nurses and dialysis technicians.
- The dialysis machine pumps blood from the body to the dialyzer through flexible blood tubings. Heparin infusion or continuous saline flushing is done to prevent clotting of blood.
- The dialyzer (artificial kidney) is a special filter through which blood flows which removes extra fluids and waste products. Dialyzer purifies blood with the help of special solution called dialysate which is prepared by a dialysis machine.
- Once the blood is cleaned, the machine sends it back to the body.
- Haemodialysis is carried out usually three times per week and each session lasts for about four hours.
How is the blood withdrawn for purification and returned back to the body in the process of haemodialysis?
The three most common types of vascular access for haemodialysis are central venous catheters, native arterio-venous (AV) fistulas and synthetic grafts.
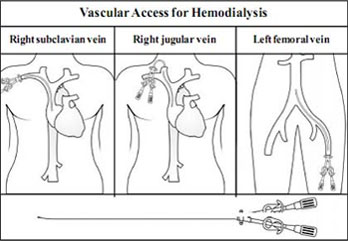
1. Central Venous Catheter
As soon as the decision to start immediate haemodialysis is made, a vascular access or central venous catheter has to be inserted. The vascular access will allow the blood of the patient to leave the body and be brought to the artificial kidney or dialyzer to be cleaned or filtered.
This method of vascular access is ideal for short-term use until a fistula or graft is ready.
A catheter is inserted into a large vein in either the neck, chest, or leg near the groin (internal jugular, subclavian and femoral veins respectively). With this catheter more than 300 ml/min blood can be withdrawn for dialysis.
Catheters are flexible, hollow tubes with two lumens. Blood leaves the patient’s body passing through one lumen, enters the dialysis circuit, and is returned to the body via the other lumen.
Venous catheters are immediate but temporary accesses for haemodialysis especially on emergency cases.
Two types of venous catheters are available, tunnelled (usable for months) and non-tunnelled (usable for weeks).
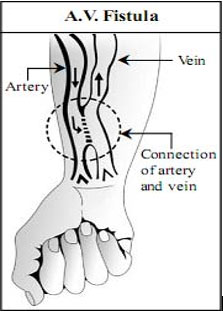
2. AV Fistula
The arterio-venous or AV fistula is the most common and the best method of vascular access for long term haemodialysis because it lasts longer, & is less likely to get clotted or inflected.
An AV fistula is created in the forearm near the wrist by surgically connecting or apposing the radial artery to the cephalic vein.
Since blood flow and pressure is higher in the artery than the vein, blood flows from the former to the latter. After a few weeks or months, the vein dilates and its walls thickens.
Such maturation of the AV fistula takes time, hence, it cannot be used for haemodialysis immediately after its construction.
For haemodialysis two large-bore needles are inserted into the fistula, one to carry blood to the dialyzer and the other to return the cleansed blood to the body.
AV fistula lasts for many years if maintained well. All usual daily activities can be easily performed with the hand having AV fistula.
Why does AV fistula need special care?
- Life of a patient with CKD- ESKD depends on regular and adequate haemodialysis. The AV fistula is the permanent vascular access essential for chronic haemodialysis and is also called the lifeline for the patient on maintenance haemodialysis. Special care of AV fistula ensures adequate blood delivery for a long period.
- Large amount of blood with high pressure flows in the veins of AV fistula. Accidental injury to such dilated veins can lead to profuse bleeding, and sudden loss of blood in large volume can be life threatening. So special care is mandatory to protect veins of AV fistula.
Taking Care of AV Fistula
Proper regular care and protection of AV fistula ensures adequate blood delivery for years. Important precautions to keep a fistula healthy and working for longer period are as follows:
1. Prevent infection
Always keep the site of the fistula clean by washing the vascular access arm daily and before each dialysis treatment. It is also important to observe aseptic technique during cannulation and throughout the dialysis process.
AV fistula is the “lifeline” in patients of CKD, without which long term hemodialysis is not possible.
2. Protecting the AV fistula
- Use access site only for dialysis. Do not let anyone give intravenous injections, draw blood or measure blood pressure on the arm with the AV fistula.
- Avoid injury to AV fistula. Don’t wear jewellery, tight clothes or a wrist watches on the vascular access arm. Accidental injury to AV fistula can lead to sudden profuse bleeding, which can be life- threatening.
- To control bleeding, immediately apply firm pressure at the site of the bleeding with the other hand or with a tight bandage. After the bleeding is controlled, contact your doctor. Instead of making efforts to control the loss of blood, rushing to hospital for help is unwise and dangerous.
- Do not lift heavy items with the accessed arm and avoid pressure on it. Be careful; do not sleep on the arm with the A V fistula.
3. Ensure proper functioning of AV fistula
Blood flow through the AV fistula should be checked regularly by feeling the vibration (also called a thrill) three times a day (before breakfast, lunch and dinner). If the vibration is absent, your doctor or dialysis centre staff should be immediately contacted. A blood clot may have formed inside the fistula and early detection and timely intervention to dissolve or remove the clot may salvage the AV fistula.
- Low blood pressure carries the risk of failure of AV fistula, and therefore, should be prevented.
4. Regular exercise
Regular exercise of AV fistula can lead to its maturation. Even after initiating haemodialysis, regular exercise of access arm helps to strengthen the AV fistula.
5. Graft
- An arterio-venous graft is another form of long term dialysis access, which can be used when persons do not have satisfactory veins for an AV fistula or have a failed AV fistula.
- In graft method, an artery is surgically connected to a vein with a short piece of synthetic soft tube which is implanted under the skin. Needles are inserted in this graft during dialysis treatment.
- Compared to an AV fistula, AV grafts are at a high risk to develop clotting, infection, and usually do not last as long as a fistula.
To ensure adequate blood delivery and effective long term haemodialysis, special care of AV fistula is most essential.
Haemodialysis - Machine
What are the functions of Haemodialysis Machine?
- The machine prepares special dialysis solution (dialysate), which is delivered to the dialyzer for cleaning of the blood.
- The machine meticulously adjusts and monitors concentration of electrolytes, temperature, volume and pressure of delivered dialysate, which are modified as per the patient’s need. Dialysis solution removes unwanted waste products and extra water from the body through dialyzer.
- For the safety of the patient, the machine has various safety devices and alarms such as for detection of blood leakage from the dialyzer or the presence of air in blood circuit.
- Computerized models of haemodialysis machine with display of various parameters on front screen and different alarms provide convenience, accuracy and safety to perform and monitor dialysis treatment.
The haemodialysis machine, with the help of dialyzer, filters blood and maintains fluid, electrolyte and acid base balance
Haemodialysis - Dialyser
What is the structure of the dialyzer and how does it purify blood?
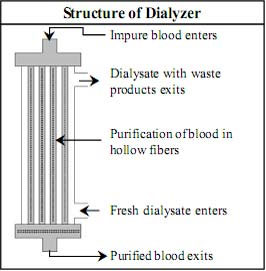
Structure of dialyzer
In the process of haemodialysis , dialyzer (artificial kidney) is a filter where purification of blood occurs.
Dialyzer is about 20 centimetre long and 5 centimetre wide clear plastic cylinder which contains thousands of tube-like hollow fibres composed of synthetic semi - permeable membrane.
These hollow fibres are connected with each other at upper and lower end of the cylinder and form the “blood compartment.” Blood enters in the “blood compartment” of hollow fibres from the opening or blood port from one end and exits from the other end after purification.
Dialysis solution enters from one end of dialyzer, flows around the outside of the fibres (“dialysate compartment”) and exits from the other end.
Process of haemodialysis
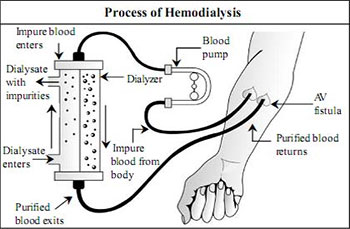
Purification of blood in dialyzer
In Haemodialysis, blood flows out from the patient through the vascular access and blood tubings into one end of the dialyzer where it is distributed into thousands of capillary-like hollow fibres. The dialysis solution enters from another port and flows around these fibres in the “dialysate compartment” of the dialyzer.
Every minute, about 300 ml of blood and 600 ml of dialysis solution continuously flow in opposite directions within the dialyzer. The semi-permeable membrane of the hollow fibres which separates the blood and the dialysate allows removal of waste products and excess fluid from the blood to the dialysate compartment.
Blood exits from the other end of dialyzer after purification. Dialysis solution with toxic substances and excess fluid which are removed from the blood exits from the end of dialyzer from which blood enters.
In haemodialysis, the blood volume of the patient circulates and passes through the dialyzer about twelve times. After four hours of treatment, blood urea and serum creatinine levels are reduced substantially, excess fluids are removed and electrolyte levels are corrected.
What is dialysate and its function in Haemodialysis?
- The dialysate (dialysis solution) is the special fluid used in haemodialysis to remove waste and extra fluid from the blood.
- The composition of the standard dialysate resembles normal extracellular fluid, but depending on the need of the patient, its composition can be modified.
- The dialysate is prepared by manufacturer by mixing about 30 parts of highly purified water with one part of dialysate concentrate.
- The dialysate concentrate is a special fluid that is commercially available, which contains electrolytes, minerals and bicarbonate.
- The water used to make the dialysate is purified sequentially by a sand filter, a charcoal filter, water softener, reverse osmosis, deionization and ultraviolet filtration. The product of these processes is water that is essentially free of dust, suspended impurities, chemical impurities, minerals, bacteria and endotoxins.
- This careful purification of water and subsequent monitoring of its quality is essential to protect patients from the risk of contaminants in the water. Each patient is exposed to about 150 litres of water during each haemodialysis session.
Where is Haemodialysis done?
Haemodialysis is usually done in hospitals or dialysis centres by trained staff under the supervision of a doctor. In a few stable patients, it may be done at home. Home haemodialysis requires proper training of the patient and family members, adequate space and financial resources.
Is haemodialysis painful? What does the patient do during dialysis?
The haemodialysis procedure is not painful. There may be slight pain experience during intravenous needle insertion when the blood tubings are connected to the patient at the start of the procedure. This outpatient requires the patient to go to the hospital or dialysis centre thrice a week and going home afterwards. During the treatment, patients rest, sleep, read, listen to music or watch television. They may even take light snacks and hot or cold drinks during this time.
What are the common problems during haemodialysis?
Common problems during haemodialysis include low blood pressure (hypotension), nausea, vomiting, muscle cramps, weakness and headache. These adverse events may be avoided by appropriately accessing the haemo-dynamics and volume status before the dialysis session. Weight gain in between sessions should be monitored, as well as serum electrolytes and haemoglobin levels.
Changes in dialysate composition helps correct electrolyte imbalance and during the process of Haemodialysis.
Haemodialysis - Advantages and Disadvantages
Advantages of haemodialysis:
- Since treatments are done by trained nurses or technicians, patients are subjected to less burden of caring for themselves. Some patients find haemodialysis more comfortable and less stressful than peritoneal dialysis.
- Haemodialysis is faster and more efficient per unit time than peritoneal dialysis.
- Haemodialysis centre provides a platform to meet and interact with other patients with similar problems. Such interaction can reduce stress and the patient can enjoy company of fellow patients.
- Haemodialysis is usually done for 4 hours, three times a week. Between treatments, patient may enjoy “free time”.
- Patients avoid the risks of peritonitis and exit-site infections.
- In some countries, haemodialysis is less expensive than peritoneal dialysis.
The main advantages of haemodialysis are safety, effectiveness and comfort.
Disadvantages of Haemodialysis:
- Inconvenience and time lost for regular travel to the haemodialysis center especially when the latter is located far from home.
- Due to fixed schedule for haemodialysis, the patient has to plan all activities around the treatment schedule.
- Frequent needle pricks and insertion during treatments can be painful. There are some measures like application of topical anaesthetics to diminish the pain in some cases.
- Dietary restrictions of fluid, salt, potassium and phosphorous still have to be observed. Patients need to adhere to these limitations .
- There is a risk of contracting blood-borne infections like Hepatitis B and C.
Do’s and Don’ts for Haemodialysis Patients
- Patients with ESKD on maintenance haemodialysis need regular treatments, usually thrice weekly. Skipping or missing treatments are deleterious to health.
- Haemodialysis patients have to observe proper dietary restrictions. Fluid, salt, potassium and phosphorous restriction have to be observed. Protein intake should be regulated upon the advice of the doctor or renal dietician. Ideally, weight gain between dialysis should be kept at 2 to 3 kgs. (4.4 to 6.6 lbs) only.
- Malnutrition is common in patients on haemodialysis and leads to poorer outcomes. A referral to a dietician with the supervision of the doctor is necessary to maintain enough caloric and protein intake to maintain adequate nutrition.
- Patients on maintenance haemodialysis may need to be supplemented with water-soluble vitamins like vitamins B and C. They should avoid over-the-counter multivitamins which may not contain some required vitamins, may contain inadequate levels of some required vitamins, or may contain vitamins that may be harmful for CKD patients such as vitamins A, E and K.
- Calcium and vitamin D may be supplemented, depending on blood levels of calcium, phosphorus and parathyroid hormone.
- Lifestyle changes are mandatory. General measures include smoking cessation, maintenance of ideal weight, regular exercise and limitation of alcohol intake.
The main disadvantage of haemodialysis is the need to visit a centre three times a week.
When to contact a doctor?
When should a patient on haemodialysis consult a dialysis nurse or doctor?
The patient on haemodialysis should immediately consult a dialysis nurse or doctor in cases of :
- Bleeding from AV fistula site or catheter site.
- Disappearance or absence of vibration, bruit or thrill in the AV fistula.
- Unexpected weight gain, significant swelling or breathlessness.
- Chest pain, very slow or fast heart rate.
- Development of severe high blood pressure or low blood pressure.
- Confusion, drowsiness, unconsciousness or convulsions.
- Fever, chills, severe vomiting, vomiting of blood or severe weakness.